Estimated read time: 5-6 minutes
This archived news story is available only for your personal, non-commercial use. Information in the story may be outdated or superseded by additional information. Reading or replaying the story in its archived form does not constitute a republication of the story.
BLUFFDALE — Katy and David Monson’s family vacation to Arizona last summer took a wild turn when they found what they thought looked like a bite mark on their son’s body.
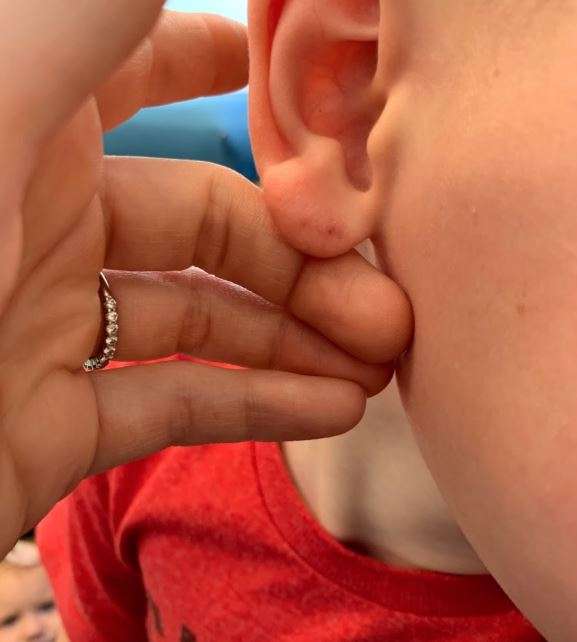
“I noticed as we were getting my son dressed that he had some weird piercings on his ear,” Katy explained.
After the parents found bat droppings in their cabin, they decided to take their son to the doctor back in Utah.
“He measured the earmarks and he said that matches a bat bite,” Katy said.
Knowing that rabies — a 100% fatal disease — can follow a bat bite, the doctor advised the whole family of five to get treated immediately.
“If you show any symptoms, it’s too late. You’re done,” David said.
High Cost Of Treatment
The doctor warned Katy the rabies treatments would be expensive. It requires a series of four vaccines and a dose of immunoglobulin. The immunoglobulin dosage depends on a person’s weight, so is considerably more expensive for adults than children.
A nurse at the Utah Department of Health referred the family to Intermountain Medical Center because that hospital’s emergency room would be able to administer the vaccine to both the adults and children.
After the initial round of shots, Katy started shopping around for the follow-up vaccines.
“I actually ended up doing a ton of research to try to find the most affordable place within our network,” she said.

The young mother thought the treatment might cost $3,000-4,000 per family member. She wasn’t prepared for the massive bills that followed. The total cost was over $51,000.
Even with insurance, the Monson family still had to pay more than $13,000 — their out-of-pocket maximum for the year.
“The overcharging was just absurd,” David said. “I am happy to pay for the treatment. But like, let’s be reasonable, right? It’s just kind of a frustrating situation.”
The Monsons called the KSL Investigators to find out why the treatments were so expensive.
Chargemaster explained
Beginning Jan. 1, 2019, the federal government required every hospital to publicly post a price list, called a chargemaster, with the intent of providing price transparency and help consumers shop around for healthcare. The lists should show customers what they charge for all services — including procedures, vaccines or a prescription administered on-site. This chargemaster is usually listed on the hospital’s website.
So, what happens when what’s on that price list is nowhere near what actually shows up on the bill?
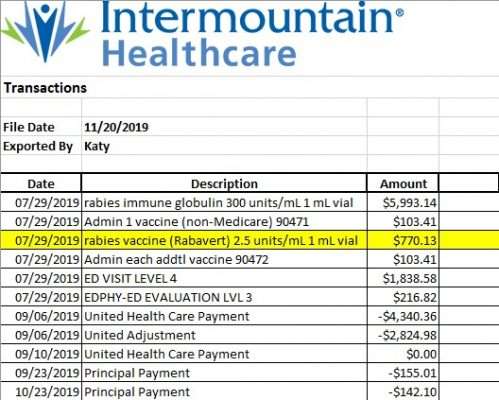
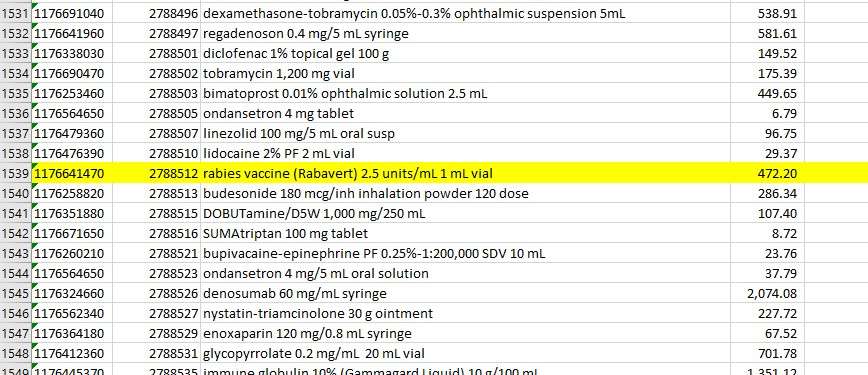
The 2019 chargemaster for Intermountain Medical Center — where the Monson family went for treatment — lists the rabies drug RabAvert at $472.20 per shot.
However, they were charged nearly $300 more than that — $770.13 total per shot.
When the KSL Investigators reached out to Intermountain Healthcare to find out why the bill was different than the posted rate, they declined an on-camera interview, but in an emailed statement said, “a review of the billing for treatment of rabies exposure for this family was conducted and the billing is correct.”
Additionally, Intermountain’s spokesperson said the “cost is driven by drug pricing set by pharmaceutical companies.” With this drug, he said the high price was “fueled by national shortages and other factors.”
The KSL Investigators next reached out to drugmaker GlaxoSmithKline (GSK), which makes RabAvert. GSK told KSL their maximum price in 2019 was $337 per dose.
When we again reached out to Intermountain for clarification, the KSL Investigators were told “there are underlying costs of running a hospital,” such as keeping the lights on and administrative costs, which they said may explain the price difference.
Intermountain also pointed out that in the Monson family’s case, their insurance covered $400 per dose, so their final out-of-pocket cost was $370 per shot, less than the listed price.
The Monsons said they’re not sure what else they could have done to lower their bill.
“I was on the phone non-stop just trying to like wheel and deal and find the best prices. I felt like we were making the best possible decision. And until it all shakes out, you don’t know what you’re getting,” Katy said.
No enforcement on price lists
Norm Thurston has spent his career studying health care costs. He is the Executive Director of the National Association of Health Data Organizations and a state lawmaker.
“It should be in the general ballpark, so you have at least some confidence that something like that is what you’re going to see on your bill at the end of your treatment,” he said. “If people are not being forthcoming and realistic about those prices, then that frustrates the purpose of why transparency can be helpful.”

He equates that cost to the sticker price when buying a car. You’d never expect to pay more than that price.
“The sticker price gives you a starting point for negotiation, but you should expect to negotiate something lower than that or get something lower than that,” Thurston explained.
However, Thurston said while federal law requires hospitals to post price lists, nothing says they have to stick to those prices. It’s something Thurston said the federal government is still trying to figure out.
In an email, Intermountain’s spokesperson wrote, “public chargemasters are posted and updated annually, and pricing may vary during the year. As noted, ‘Prices listed are effective as of Jan. 1, 2019. Actual charges may vary.’ With 2,800 medications in use at Intermountain Medical Center and due to continual well-publicized gyrations in the pharmaceutical industry, prices will vary during the year based on the hospital’s cost to acquire the medications.”
Centers for Medicare and Medicaid told us hospitals are only required to update their price lists once a year. Beginning Jan. 2021, hospitals and insurers will be required to give even more information for health care estimates.
The new rule also gives the law an enforcement mechanism. But as the rule is currently written, it appears enforcement only applies to hospitals not posting the list. It is unclear if hospitals will be required to adhere to those prices.
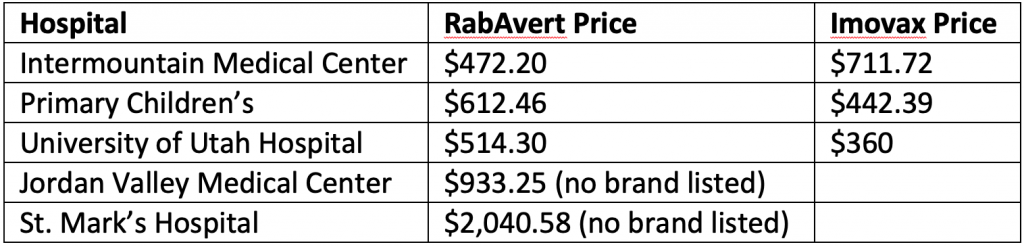
The listed price for RabAvert and Imovax (another rabies drug) varies widely among hospitals in the Salt Lake Valley. Here are the prices listed on their 2019 chargemasters: