Estimated read time: 8-9 minutes
This archived news story is available only for your personal, non-commercial use. Information in the story may be outdated or superseded by additional information. Reading or replaying the story in its archived form does not constitute a republication of the story.
SALT LAKE CITY — The running average of people testing positive for COVID-19 compared to the number of people tested is plummeting, and that's a good sign after it surged to record levels at the end of 2020.
Utah's seven-day COVID-19 positivity rate fell below 20% last week for the first time since it was 19.99% on Oct. 26, 2020; the rate is backdated to account for the results of all tests conducted. As of Jan. 15, the most recent data available, it was at 19.03%, according to a Utah Department of Health update Thursday.
Of course, that doesn't mean the coronavirus pandemic is over — or an end to new hospitalizations — but it offers hope that the spread of COVID-19 across Utah might be declining. Experts offered a word of caution, however, that differences in testing types may also be influencing the apparent decrease in positivity rate.
The positivity rate roller coaster
Public health experts from all over the state have pinpointed test positivity as one of the key data points when it comes to the state of new cases, especially when the number of tests conducted daily isn't constant, which can impact the number of new cases.
The holiday season resulted in a downturn of tests conducted and the return to school is expected to lead to a rise in new testing. Even days of the week aren't equal when it comes to testing rates. The state often reports fewer tests conducted on weekends.
The positivity rate helps provide a more stable number when it comes to transmission rates.
In the world of epidemiology, a higher percentage means more likelihood that a large number of people aren't accounted for in testing.
When Utah experienced its first real uptick of COVID-19 cases after Memorial Day last year, Utah's positivity rate remained close to 10%. In fact, it remained about the same throughout June, July and August. It wasn't until early September, which is when a surge of new cases was reported, that the positivity rate moved upward closer to 15%. It surpassed 15% on Oct. 11 and 20% by the end of October, according to state health department data.
While a decline in testing led to a decline in new cases over the holidays, the seven-day positivity rate didn't fall below 20%. It indicated that many people who may have been sick weren't getting tested.
Put together on a graph, the holidays produced a roller coaster of results.
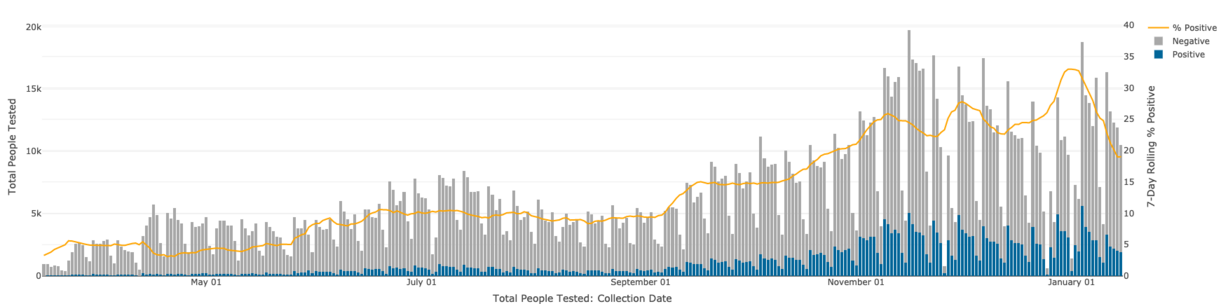
These were the highs and lows of that stretch:
- Oct. 26: 19.99%
- Nov. 10: 25.90%
- Nov. 23: 22.25%
- Dec. 1: 27.77%
- Dec. 13: 22.63%
- Jan. 1: 32.98%
- Jan. 14: 18.97%
The rate reached peaks on Nov. 10 and Dec. 1 before the state reported declines and rises. The state's current positivity maximum rate peak happened on Jan. 1, when it was 32.98%. It's steadily fallen since. It fell every day for the first two weeks of the year to 18.97% on Jan. 14. Thursday's update of 19.03% on Jan. 15 is the first time so far that the rate has increased in 2021 — even if it was just 0.06 percentage points.
There are signs it could fall a bit lower. Some of the state's unofficial rates between Jan. 15 and Thursday show a rate less than 19%. Johns Hopkins University's Coronavirus Resource Center uses a less-backdated rate and listed Utah at 17.28% on Thursday.
The center also listed Utah as having the 10th-highest rate among states even with the decline. Idaho currently leads all states with a rate of 36.52%. The U.S. average was 9.8% — down from 13.6% at the start of the month.
All of the declines are a step in the right direction.
What's causing the decline?
The Utah Department of Health issued a statement to KSL.com on Thursday, acknowledging the decline could be a result of "a variety of reasons" including a rise in testing.
"We are testing more people now and have been promoting a 'testing surge' across the state since the beginning of the year in anticipation of schools/universities reopening," the statement read, in part. "As you increase the number tested, it increases the denominator and will lower the percent positivity."
Public health experts find themselves "cautiously optimistic" when it comes to the data. Is the decline caused by the virus leaving Utah or is it due to a switch in testing methods?
If it's the former, then a lower positivity rate can likely signal a decline in new cases, said Dr. Eddie Stenehjem, during a virtual question and answer session last week.
"That's a good sign, that's a good trend," he said, of the test positivity rate.
Earlier this month, Dr. Todd Vento, another Intermountain Healthcare infectious disease physician, explained that an increase in testing doesn't always result in a change in positivity rate as a whole. It could, however, help give infectious disease experts a better idea of how the virus is spreading in the state.
If the recent positivity rate decline is caused by the latter, then it could mean issues with all sorts of COVID-19 data. In an interview with KSL.com on Thursday, Vento said there remains a consistent load of testing volume but there was a spike in a switch from PCR testing to antigen testing recently.
Antigen testing is a better tool when handling large groups of asymptomatic individuals who need to be tested — like mass testing college students — but it comes with a higher likelihood for a false negative response. Therefore, it's possible that it could drive down the test positivity rate even if the virus itself isn't leaving the state.
"It's well known that you can have some degree of false negativity or false negatives, more so with the antigen tests," he said. "If we've increased the number of antigen tests we've (used) we would find a decreased number of positives who still might be positive."
The sharp decline over a two-week span is why Vento believes it's possible that "a little bit of both" is currently happening. That is, there's a possibility that the true positivity rate is somewhere between 19% and 33%. It's why he theorized it's possible that the state could issue positivity rates reflecting both PCR and antigen testing when releasing future results.
"I think the thought in local circles in discussions with the health department is there might be some overall decrease but it's hard to see how much of it is coming because of doing more antigen testing, which might be diluting out the overall positivity rate a bit," he added.
It may take another couple of weeks to determine if there's a significant differential in rates between the two forms of testing.
Not out of the woods just yet
Even if Utah's positivity rate has truly dropped below 20% for the first time since late October, health experts warn it's too high. The recommended goal is under 5%, which Utah last reported on May 20, 2020.
It's worth noting that Utah isn't alone in this struggle. Johns Hopkins reports that only six states (Alaska, Connecticut, Hawaii, North Dakota, Rhode Island and Vermont) and the District of Columbia had rates below 5% on Thursday.
One of the primary transmission concerns, outside of the high rate, is that a variant of the virus first found in the United Kingdom that's known to spread faster than the originally known strain was recently detected in Utah. The Centers for Disease Control and Prevention said models project that the U.K. variant will be the dominant strain in the U.S. by March. The mutated virus currently doesn't pose a known threat to vaccination efforts but could lead to an uptick of new cases and hospitalizations before most people will have access to a vaccine.
The decline in positivity rate now also doesn't provide a snapshot of Utah's current hospital issues.
Health department data shows that the seven-day average of new COVID-19 hospitalizations rose in the first week of 2021. It climbed from 66.6 new hospitalizations per day on Dec. 25 to 87.4 on Jan. 8 — not far from the current peak of 93.7 on Nov. 19. As of Jan. 15, it's at an average of 78 new hospitalizations per day.
There are still 529 Utahns currently hospitalized as a result of COVID-19, according to Thursday's update. That's compared to 127 on Sept. 1, 2020, which was just before the fall surge in cases and hospitalizations.
Intensive care unit utilization for referral centers was still dangerously high at 94% and 91% statewide. The utilization warning is 72% and the threshold is 85% for reference.
The number of deaths from COVID-19 is also still rising even if not at the highest rates experienced at the end of 2020. Thirty more Utahns died as a result of COVID-19, the health department reported Thursday.
It's why health experts say the positivity rate decline is encouraging but doesn't signal an end to public safety measures.
"Mask wearing, staying home when sick/symptomatic, physical distancing, and washing hands are all effective in slowing the spread and as these behaviors become more of the norm, we will see fewer transmissions," state health officials added in the department's statement.
Vento agreed.
"You think of all the factors going on. They're changing some of our testing techniques ... but we're also going to have more of this virus strain that's more easily transmitted," he said, adding that if what happened with the new COVID-19 variant in the U.K. happens throughout Utah that there could be an uptick of new cases, which would lead to hospitalizations and deaths before people can receive the COVID-19 vaccine.
"(It's) why it's so much more critical now that people be more aggressive with their masks and their distancing and avoiding gatherings," Vento said. "Because the danger is that if we increased the chance of a virus to mutate by just growing and spreading ... eventually we could end up with a virus that could be resistant to our vaccine."









