Estimated read time: 5-6 minutes
This archived news story is available only for your personal, non-commercial use. Information in the story may be outdated or superseded by additional information. Reading or replaying the story in its archived form does not constitute a republication of the story.
SALT LAKE CITY — Jamie Clinton-Lont well remembers the day in 2005 she got a call from the husband of her 44-year-old patient to report she had died of an overdose.
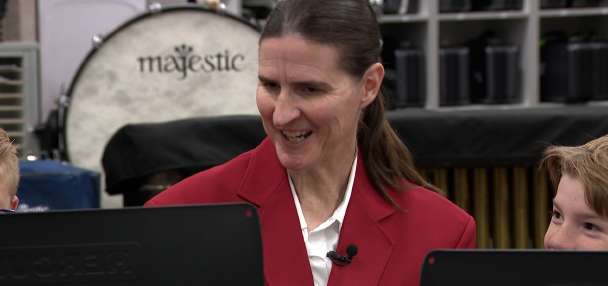
"He said 'Jamie, my wife is gone,'" remembers Clinton-Lont, a nurse practitioner and founder and director of an opioid education and monitoring system at George E. Wahlen VA Medical Center in Salt Lake City. "It's not easy to talk about. It bothers me today."
Clinton-Lont calls that day a "turning point" in her understanding of the risks of opioids — a shift in perspective that "changed my practice."
Since then, she said, she has grown to realize that many other medical professionals also wrestle with the fallout of the opioid addiction crisis as it affects their patients.
"(They are) left with something that carries with them their whole life," Clinton-Lont told a group of health providers, social workers, government officials, educators, mental health experts and others Wednesday at Utah State University Extension's Opioid Health and Wellness Summit in downtown Salt Lake.
The inaugural conference coincides with Utah State University Extension's program called Health Extension Advocacy, Research & Teaching, which launched in the spring with the hiring of five new faculty members "to provide credible health and wellness resources" across the state.
"These professional practice assistant professors will be based in some of the communities hit hardest by the opioid crisis in Utah," university spokeswoman Julene Reese explained in a release.
Utah State University Extension has a unique role in promoting educational resources throughout the state, including rural areas where community resources are less abundant, so it made sense for it "to put skin in the game and try to help" combat the scourge of opioid addiction, said university extension Vice President Kenneth White.
"Some of our more rural communities don't necessarily have access to the resources and programming" addressing the risks of opioids and addiction prevention, White said.
"That's where we can help," he added.
Clinton-Lont referenced data pointing out Carbon, Emery and Grand counties, as well as downtown Ogden, as hot spots for opioid abuse in Utah. The state has the seventh highest fatal overdose rate in the country.
"These need to be our rural focus areas," she said.
Kathy Donathan, health education specialist for the Southeast Health District that oversees the three counties Clinton-Lont listed, implored conference goers, "We are fighting a big fight and we want your help."
The problem is people are going to the streets to get the pill they think they can't get through their doctors.
–Jamie Clinton-Lont
"It's a beautiful place to raise a family and to live, (but) we are dying" from opioid abuse, Donathan said during a panel discussion. "We need your help. We have no detox center, no recovery centers."
Brian Besser, special agent in charge for the Drug Enforcement Administration in Utah and another panelist at the summit, said that besides the need for resources, the state also needs to see a cultural shift in how to respond to those who fall into addiction and talk about the issue openly.
Besser cited an incident in his own neighborhood, in which he found out well after the fact that the adult son of his friends in the area had died of an overdose in their home.
"What was interesting to me was nobody talked about it. It was so quiet. I found out by accident," he said.
Besser said that in the fight against opioid addiction, "one of the greatest enemies right now that I see is shame."
"That is what's killing people right now, especially in this state, because people don't feel at liberty to discuss the problems that they're dealing with," he said.
Related story:
Clinton-Lont shared the same sentiment in her remarks Wednesday, saying medical providers and public health officials ought to be "the change agent for how we talk about addiction."
She also urged attendees that "keeping this topic on the table, and not just when we have an epidemic, is very important."
"We need to look at our patterns and change for the future," Clinton-Lont said. "When it becomes less of a hot topic, we still need prevention."
Clinton-Lont said historically in American health care, medical professionals and patients alike have "always kind of wanted to have a quick fix," which made the country susceptible to rushing headlong into "the latest, greatest drug" in the 1990s: opioids.
"'It will take your pain away it's safe and it's non-addictive' is what we were taught," she said.
By about 2010, many doctors started to "cut back a little bit" due to prescription painkillers' dangers becoming more and more clear, she said, but that couldn't ultimately hold back the tide of long-term addiction many were suffering from, and increasing numbers of Americans turned to street opioids such as heroin.
In recent years, the use of even more overpowering and dangerous street opioids like fetanyl and carfentanil has been more prevalent, according to Clinton-Lont.
Currently, people who think they are buying something with roughly the street equivalent potency of certain prescription painkillers may in fact be getting a substance laced with carfentanil, many thousands of times more powerful, which is extremely dangerous, she said.
"The problem is people are going to the streets to get the pill they think they can't get through their doctors," Clinton-Lont said. And because of the much more powerful dose, "they're dying within seconds."
Ideally, doctors need to have straightforward conversations with their patients about risks before they ever open the door to opioid addiction, she said.
"Even though it may feel a little bit ... uncomfortable, it is what is needed," Clinton-Lont said.
Correction: An earlier version incorrectly identified the vice president of Utah State University Extension. His name is Kenneth White, not Kenneth Harwood. Email: blockhart@deseretnews.com Twitter: @benlockhartnews