Estimated read time: 7-8 minutes
This archived news story is available only for your personal, non-commercial use. Information in the story may be outdated or superseded by additional information. Reading or replaying the story in its archived form does not constitute a republication of the story.
SALT LAKE CITY — This week's health briefs include a better way to predict mortality, the health trajectory that hints diabetes may be coming, and two questions: What level of "good" cholesterol leads to dementia? And should new dads be screened for postpartum depression?
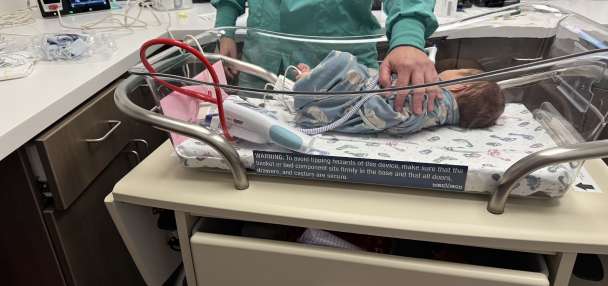
Dads and postpartum depression
New moms aren't the only ones who suffer postpartum depression. A pilot study at the University of Illinois Chicago finds that dads can also develop the sometimes debilitating condition and should be screened, too.
"A lot of dads are stressed. They're scared. They're struggling with balancing work and parental and partner responsibilities," said Dr. Sam Wainwright, the study's lead author. "Men are often not doing well, but no one is asking them about it."
The research notes that fathers' and mothers' mental and physical health are often intertwined and called addressing the health of fathers a potential "powerful untapped tool" to help solve the ongoing national maternal health crisis.
In a small study, published in the journal BMC Pregnancy and Child Birth , 24 dads were screened at UI Health's Two-Generation Clinic, using the tool used to screen moms for postpartum depression. A third of them screened positive.
The clinic itself was created because low-resource mothers of color often don't take care of their own health, but may be careful to ensure their children see a doctor, Wainwright said. The clinic offers moms primary care at the same time, but not dads. However, when the staff asked dads how they were doing, they often heard the men were not doing really well.
"Those conversations also spurred a larger research project that Wainwright has begun to learn more about the experiences of dads, especially as related to their mental and physical health. Perhaps well-baby visits aren't the only place to reach dads, he said, so he's started talking to fathers-to-be in the obstetrics waiting area, too. He's also asking to screen dads for conditions like high blood pressure during these conversations," per a UIC Today release .
While the study said dads self-reported low rates of stress and preexisting mental health conditions, a third tested positive for postpartum depression or suicidal ideation. They also found 26% of them didn't have health insurance and more than half (54%) didn't have a primary care physician.
The researchers said concerns that might otherwise have gone unnoticed were found and for some the screening was "an effective tool to prompt their subsequent engagement with general health care. This pilot is a step toward incorporating the health of fathers into models for supporting the health of families."
Related Story
Does mass or body composition best predict mortality?
An individual's waist-to-hip ratio seems to be a better predictor of mortality than using body mass index, per a study in JAMA . The research is based on data from 387,672 white British participants in the UK Biobank, the data analyzed twice.
The two methods both assess fat distribution. But the researchers said that the second analysis "suggested that the association between waist-to-hip ratio and all-cause mortality is likely causal," per an article on JAMA Network Online.
There's growing evidence that body mass index, or BMI, alone — a calculation that uses a person's height and weight but doesn't take into account whether weight is muscle or fat or if one has a sturdy or petite frame, for instance — is not the best predictor of death.
A July study in PLOS ONE said associations between BMI and death have been inconsistent. It noted that past BMI studies have also typically used data from the 1960s through the 1990s "that predominantly include non-Hispanic white men and women."
In the newer comparison of the two measures, the scientists concluded that the waist-to-hip ratio "had the strongest and most consistent association" with mortality, regardless of BMI. They said that's what clinicians should focus on when making recommendations about diet and weight and health.
Illnesses preceding Type 2 diabetes diagnosis
More than a third of patients diagnosed with Type 2 diabetes had recently also been diagnosed with high blood pressure and respiratory tract infection. As many as 1 in 5 had been seen for a heart condition or ear, nose and throat infection.
Researchers from the United Kingdom said their findings, presented this week in the poster session at the Annual Meeting of the European Association for the Study of Diabetes, suggest a significant uptick in those common conditions could prompt concern about Type 2 diabetes and lead to earlier diagnosis. Findings were previously published in Diabetologia , a peer-reviewed publication.
"These novel insights into the onset and natural progression of Type 2 diabetes suggest an early phase of inflammation-related disease activity long before any clinical diagnosis of Type 2 diabetes is made," senior author Dr. Adrian Heald, of Manchester University, said in a news release. "These findings hint at the potential for Type 2 diabetes to be diagnosed earlier and we hope that the distinct clinical trajectory could become a predictive tool for people at risk of the disease."
The researchers looked at longitudinal data from the Diabetes Alliance for Research in England study, noting common conditions of nearly 2,000 adults, average age 53, who were matched by age and gender. Data from 1,200 individuals with Type 2 diabetes and just over 736 without diabetes were examined, using 25 years pre-diagnosis and 25 years post-diagnosis.
Among those who were diagnosed, the share of individuals who had the earlier conditions was high. Heald said they "may serve as a precursor to the later onset of Type 2 diabetes." But he noted the study did not prove causation and there could be unknown confounding factors responsible for the result, so more study is needed.
Cholesterol and dementia
Both too much or too little high-density lipoprotein (HDL) cholesterol — the "good" kind — could create a small increased risk for dementia in older adults. That's from a study in Neurology , the medical journal of the American Academy of Neurology . This study does not prove HDL levels cause dementia, but shows an association.
"Previous studies on this topic have been inconclusive and this study is especially informative because of the large number of participants and long follow-up," said study author Maria Glymour, of Boston University, said in a written statement. "This information allowed us to study the links with dementia across the range of cholesterol levels and achieve precise estimates even for people with cholesterol levels that are quite high or quite low."
Related Story
The study included 184,367 people from the Kaiser Permanente Northern California Health Plan, average age 70, who did not have dementia when the study began. Besides answering questions about their health behaviors, their cholesterol levels were measured in routine health care visits about 2.5 times in two years. They were then followed within the Kaiser health care system via electronic health records for an average of nine years. In that time, 25,214 developed dementia.
Per the release, "The average HDL cholesterol level was 53.7 milligrams per deciliter (mg/dL). Healthy levels are considered to be above 40 mg/dL for males and above 50 mg/dL for females. Participants were divided into five groups based on their HDL cholesterol levels. People with the highest levels of HDL cholesterol had a 15% higher rate of dementia compared to those in the middle group. Those with the lowest levels had a 7% higher rate of dementia compared to those in the middle group."
The researchers controlled for other factors that can increase risk of dementia, including alcohol intake, hypertension, cardiovascular disease and diabetes.
They found "only a slight association" between low-density lipoprotein — so-called "bad" cholesterol" — and dementia risk.
Because people volunteered to be in the study, they may not be representative of the larger population.